The Business Case for Breastfeeding tells us that 80 percent of mothers stop breastfeeding within the first month of returning to work (Cardenas & Major, 2005). Unfortunately, research on returning to work and breastfeeding is limited. There are several critical factors for supporting breastfeeding in employed mothers that I have identified in the literature and my clinical practice. Despite the dire statistics, mothers in my practice were actually doing well. None of them were quitting breastfeeding in the first month of returning to work. Providing accurate information about how breast milk supply works and how to move their breast milk, along with a little social/emotional support seemed to help my clients keep breastfeeding despite the occasional difficulty. We have a number of ways to help you be successful! Read on and check out our new phone app, iLactate: Back to Work!
The Business Case for Breastfeeding tells us that 80 percent of mothers stop breastfeeding within the first month of returning to work (Cardenas & Major, 2005). Unfortunately, research on returning to work and breastfeeding is limited. There are several critical factors for supporting breastfeeding in employed mothers that I have identified in the literature and my clinical practice. Despite the dire statistics, mothers in my practice were actually doing well. None of them were quitting breastfeeding in the first month of returning to work. Providing accurate information about how breast milk supply works and how to move their breast milk, along with a little social/emotional support seemed to help my clients keep breastfeeding despite the occasional difficulty. We have a number of ways to help you be successful! Read on and check out our new phone app, iLactate: Back to Work!
Breastfeeding is Going Well Before Returning to Work

One critical factor for success is having the mother be good at breastfeeding before she returns to work. We know that breastfeeding becomes less work (and generally easier) for most mothers at about six to seven weeks (Mohrbacher & Kendall-Tackett, 2010). If breastfeeding isn’t going well or a mother goes back to work before six to seven weeks, she is more likely to be unsuccessful with this transition. If a mother is struggling with pain, has a baby who doesn’t feed well at the breast, or her milk supply is low when she returns to work, she is doubly challenged from the get go! Providing a plan to address these issues along with hope, accurate information and support can help mothers continue breastfeeding even as they return to work.
 Support from an IBCLC
Support from an IBCLC
The support and information an IBCLC can provide are critical for a mother. Many mothers don’t have anyone in their lives who understand or care about why they are even trying to continue to breastfeed and work. IBCLCs do care. We want her to be able to meet her breastfeeding goals. Together we can help shift those low statistics of working and breastfeeding success.
Success at Milk Removals
 Another critical factor for success is how well the mother is removing her milk when separated from her baby. Most of my clients use a standard, personal use, double electric breast pump. But as we know, not all pumps are created equal. Some work well, some don’t work as well. Using a brand of pump that has a good vacuum, different size breast shields (so important!), and variable speeds will increase her chance of success. At the same time, if a breast pump has all these things and she is still not getting out her breast milk, IBCLCs have to get creative. Maybe she needs to try a different brand of pump, rent a hospital grade pump, use a hand pump, or hand express? Watching a mother pump is important. Test the vacuum. Make sure her shields fit well (Meier, 2004; Prime et al., 2010). Many mothers have no idea that different size breast shields even exist!
Another critical factor for success is how well the mother is removing her milk when separated from her baby. Most of my clients use a standard, personal use, double electric breast pump. But as we know, not all pumps are created equal. Some work well, some don’t work as well. Using a brand of pump that has a good vacuum, different size breast shields (so important!), and variable speeds will increase her chance of success. At the same time, if a breast pump has all these things and she is still not getting out her breast milk, IBCLCs have to get creative. Maybe she needs to try a different brand of pump, rent a hospital grade pump, use a hand pump, or hand express? Watching a mother pump is important. Test the vacuum. Make sure her shields fit well (Meier, 2004; Prime et al., 2010). Many mothers have no idea that different size breast shields even exist!
Positive Associations to Help Her “Feel the Love” for Her Pump

Make sure she is feeling the love for her breast pump. Without an oxytocin release, a mother is trying to pull the breast milk out of her body. With an oxytocin release, she is working in sync with her body. Her body is pushing the milk out of her breasts. This is much more effective. If she is having trouble “feeling the love,” suggest warm compresses, warm breast shields (Kent et al., 2011) and/or massage before pumping (Bolman & Witt, 2013; Bowles, 2010). She can use “hands on” pumping techniques to help get the breast milk flowing (Morton, n.d.). Also, hand expression for a minute or two on each breast after pumping can help with milk production (Morton, 2012). Some mothers find that visualizing their baby or their milk flowing helps. Others find playing Candy Crush helps! There are some hypno-pumping visualization MP4 products out there (Freeze, 2014). Have them practice breast pumping while getting a massage, eating chocolate, or watching their favorite comedy. It’s straight classical conditioning. Pair a condition with a response (think Pavlov’s dog). Clients can help train their bodies to have an oxytocin surge in response to their breast pumps.
If a mother having difficulties with her milk production, encourage her to blame her pump for lack of breast milk, not her body! If milk is not being removed effectively while she is separated from her baby, her supply will go down.
Knows the Magic Number of Milk Removals
 Mohrbacher (2012) proposes that each mother has a “magic number,” the number of times that her breast milk must be removed in 24 hours to sustain her milk supply. A “milk removal” could be a breastfeed, a pumping session, or a hand expression session. When babies are being fed too much while away from mothers they often only breastfeed from mom two or three times during a work day. Usually this is once in the morning and once before bed. If mothers are pumping three times at work, two breastfeeds + three pumps = five milk removals. Five milk removals in 24 hours is not very many. Some mothers can get away with this low number of milk removals but most can’t. Their breast milk supply starts to gradually decrease. By adding an extra pump before bed, I was helping the mother increase her milk removals that seemed to help her supply. However, perhaps it would be easier if the baby needed to nurse four to six times on a work day? This would increase a mother’s milk removals to seven to nine, which is more normal.
Mohrbacher (2012) proposes that each mother has a “magic number,” the number of times that her breast milk must be removed in 24 hours to sustain her milk supply. A “milk removal” could be a breastfeed, a pumping session, or a hand expression session. When babies are being fed too much while away from mothers they often only breastfeed from mom two or three times during a work day. Usually this is once in the morning and once before bed. If mothers are pumping three times at work, two breastfeeds + three pumps = five milk removals. Five milk removals in 24 hours is not very many. Some mothers can get away with this low number of milk removals but most can’t. Their breast milk supply starts to gradually decrease. By adding an extra pump before bed, I was helping the mother increase her milk removals that seemed to help her supply. However, perhaps it would be easier if the baby needed to nurse four to six times on a work day? This would increase a mother’s milk removals to seven to nine, which is more normal.
In order to help mothers keep track of all of this information in a fairly simple way, she will need to track just three numbers. I suggest that she total up how many ounces of breast milk she removes from her breasts in a week, how many ounces of breast milk the baby receives from the bottle in a week, and if she has a typical work week, how many times per 24 hours she moves her breast milk. I usually suggest tracking from midnight on Wednesday to midnight on Thursday.
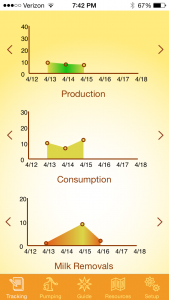
- How much milk did you pump or hand express per week?
- How much breast milk did your baby consume while away from you per week?
- How many times did you move your milk (a breastfeed, a pump, or a hand expression) from midnight Wednesday to midnight Thursday?
If clients track these numbers each week and any of these numbers starts to shift, up or down, they can catch this quickly and get help. How many times have you worked with a mother and asked when she thinks this problem started and she answers, “Well, now that I am thinking about it, about six weeks ago.” So long ago! If she is counting weekly, she can catch changes right away. Let her know she should contact you immediately if she notices a negative change.
Supportive Childcare
Working and breastfeeding success can also be at risk if her care provider does not value her breast milk or her breastfeeding relationship with her baby. Overfeeding the baby while the mother is away is a common problem. The childcare provider needs to understand that not all crying or fussiness is about food. They also need to know how to care for pumped breast milk, and how to bottle feed a baby in a breastfeeding-friendly manner by pacing the bottle feed. I actually recommend that all babies should be fed in this manner, not just breastfed babies or if there is breast milk in the bottle. Pacing the feed helps the baby control his intake and prevents overeating, which may help prevent obesity in later life.
Avoid Overfeeding at Childcare

The final stumbling block relates to overfeeding and subsequent diminished breastfeeding when moms and babies are reunited. When a baby has been overfed at child care, not only is it almost impossible to keep providing enough pumped breast milk for the baby, the baby doesn’t need to breastfeed as often from mom when they get back together. It is as if the baby is saying, “No thanks, I’m good! I had all my needed calories for day from my caregiver.” This does not hold true for all babies, but it does for many. Also, being away from mom can be stressful and tiring. Babies can sometimes sleep longer at night because of this. Between not needing to nurse because of the calorie overload during child care and sleeping longer at night, mothers can end up breastfeeding far less than they were before returning to work. I have often suggested that moms pump before going to bed if their baby was going to sleep at 8:00 PM and not feeding much during the night. This strategy appears to help improve their breast milk supply.
Summary

In my practice, I’ve found that these five things can sabotage a mother’s ability to continue breastfeeding after she returns to work: starting out with breastfeeding not working well, lack of information and support, milk removals not working well, lack of paced bottle feeding, and a mother’s daily milk removals reducing over time, are the most common culprits I have found in sabotaging a mother’s success in meeting her breastfeeding goals when returning to work. Providing information about these issues may help a mother head off trouble before it starts or at least help her quickly identify when she is moving down a slippery slope, and can greatly increase her odds of having the breastfeeding relationship she dreamed of before returning to work. Also, be sure to listen to my new podcast episode discussing the new phone app!